- Admissions
- Order Review
- Product Dispensing
- Verification
- Clinical Services
- Drug Info
| Stone, Mitchel |
| MRN: 420798 | Room: 805 | DOB: 3/21/1940 | Age: 86 | Gender: Male | Allergies: Sulfamethoxazole/trimethoprim (hives) |
| Setting | Medical ICU (MICU) | ||
| Scenario | Mr. Stone is admitted directly to the medical ICU. His clinical status continues to worsen despite an IV fluid bolus and being placed on high flow nasal cannula prior to arrival. The team is preparing to intubate the patient and place an orogastric tube post intubation. Of note, Mr. Stone has limited line access consisting of two peripheral lines. Mr. Stone has pending orders to place a central line and an arterial line. While Mr. Stone is undergoing rapid sequence intubation, using hospitalized protocols for medication selection and dosing, the intern asks you to review Mr. Stone’s case and make recommendations regarding his ongoing acute hospital problems, as well as any additional areas of optimization you may find regarding his past medical history. |
||
| Admission note taken on 02/01/26 | |||
| CC | “I am here to check-in for my hernia repair.” | ||
| HPI | Mr. Stone was transferred from Saint’s Community Hospital to Regional Academic Medical Center intensive care unit due to acute decompensation. Mr. Stone presented to Saint’s Community Hospital 3 days ago for an elective inguinal hernia repair. During Mr. Stone’s hernia repair, he became hypotensive requiring fluid administration, vasopressor therapy for 6 hours, and subsequent admission for observation. After being hemodynamically stable and having an unremarkable observation period, Mr. Stone was to be discharged today. See Clinical Notes for summary. Over the past 12 hours Mr. Stone has become increasingly short of breath and has notable sputum production. Of note, Mr. Stone was admitted to Saint’s Community Hospital two months ago for a COPD exacerbation. Saint’s Community Hospital is not affiliated with Regional Academic Medical Center, therefore details regarding his hospitalizations are limited to the transfer summary information that arrived with Mr. Stone. |
||
| PMH |
|
||
| Social History |
|
Family History |
|
| Vaccine History |
|
Surgical History |
|
| Physical Exam |
|
||
Clinical Laboratory Report
| Test Name | 02/01/26 | 12/03/25 | Range |
| Sodium (Na+) | 138 | 140 | 136-145 mEq/L |
| Potassium (K+) | 4.3 | 4.1 | 3.5-5 mEq/L |
| Chloride (Cl-) | 120 | 100 | 98-106 mEq/L |
| Bicarbonate (HCO3-) | 28 | 15 | 23-28 mEq/L |
| Urea nitrogen (BUN) | 18 | 12 | 8-20 mg/dL |
| Creatinine | 2.3 | 1.1 | 0.5-1.3 mg/dL |
| Glucose | 250 | 185 | 70-115 mg/dL |
| Hemoglobin A1c | 12 | 11 | 5.3-7.5 % |
| Calcium,Total | 8.7 | 8.6-10.2 mg/dL | |
| Phosphate | 2.4 | 3-4.5 mg/dL | |
| Magnesium | 2.4 | 1.6-2.6 mEq/L | |
| Protein, total | 6.2 | 5.5-9 g/dL | |
| Albumin | 4.5 | 3.5-5.5 g/dL | |
| Aminotransferase,aspartate (AST) | 48 | 10-40 units/L | |
| Aminotransferase,alanine (ALT) | 37 | 10-40 units/L | |
| Lactic dehydrogenase (LDH) | 80-225 units/L | ||
| Alkaline phosphatase | 30-120 units/L | ||
| Bilirubin, Total | 1.1 | 0.3-1 mg/dL | |
| Leukocytes (WBC) | 18.5 | 6.1 | 4.5-11 x103/mcL |
| Red blood cells (RBC), Male | 4.4 | 3.8-5.1 x108/mcL | |
| Hemoglobin, Male | 12.7 | 13.8 | 14-18 g/dL |
| Hematocrit, Male | 38 | 41 | 42-50 % |
| Mean corpuscular hemoglobin (MCH) | 27-33 picogram | ||
| Mean corpuscular volume (MCV) | 76-100 mcm3 | ||
| Platelets | 250 | 320 | 150-450 x103/mcL |
| International normalized ratio (INR) | 1.1 | 0.8-1.2 | |
| Prothrombin time (PT) | 11.4 | 9.5-11.3 sec | |
| Partial thromboplastin time,activated (aPTT) | 34 | 25-35 sec |
| Additional Labs: |
|
|||||||||||||||||||||||||||||||||||||||||||||
| Cultures: |
|
|||||||||||||||||||||||||||||||||||||||||||||
| Imaging Studies: |
|
| ||||||||||||||||||||||||||
Current Orders
| Medication History |
|
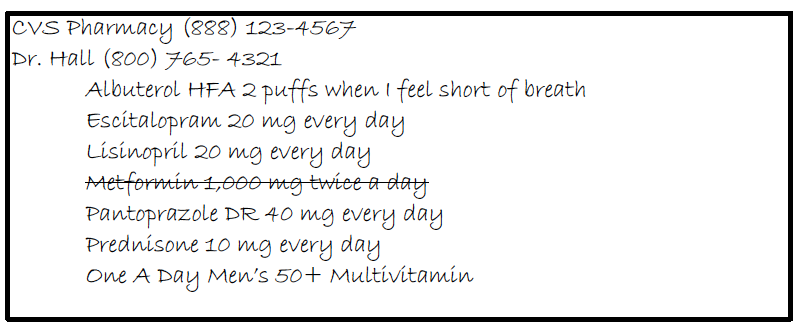
Home Medication List: verified by pharmacy on admit (02/01/26)
| Patient Name: Stone, Mitchel Date of Birth: 3/21/1940 Room#: 805 |
Allergies: |
Immunization History: |
| Community Rx Info: Rx Insurance: |
Social History: |
|
| Additional Notes: | ||
STRENGTH DF |
ROUTE FREQ |
DOSE (date/time) |
EFFECTS |
ACTION |
REASON |
|||
|---|---|---|---|---|---|---|---|---|
| Action Key: C = Continue, D = Discontinue*, H = Hold*, M = Modify* *must provide reason |
||||||||
| Medication | 02/01/26 |
| Bupropion XL 150 mg PO QD | |
| Enalapril 5 mg PO QD | |
| Escitalopram 20 mg PO QD | |
| Famotidine 20 mg PO QD | |
| Insulin, lispro 100 unit/mL SLIDING SCALE SC Q4H | |
| Metformin 1,000 mg PO BID | |
| Pantoprazole DR 40 mg PO QD | |
| Prednisone 10 mg PO QD | |
| Sitagliptin 100 mg PO QD | |
| Albuterol Sulfate 108 mcg/puff 2 puffs PO Q4H PRN PRN SOB/wheezing | |
| Dextrose 50% 25 g IV Q 30 MIN PRN PRN hypoglycemia Rate: 500 mg/kg/hr |
Clinical Notes
Medication Discharge Orders
Discharge Planning - Medication List and Instructions
| Hospital Medications | ||||||
| Medication | Instructions | Comments | Continue | Modify | Discontinue | New Rx sent |
| Previous Home Medications | ||||||
| Medication | Instructions | Comments | Continue | Modify | Discontinue | New Rx sent |
Discharge Planning - Medication List and Instructions
| Patient Name: | ||
| Admission Date: | Discharge Date: | Service: |
| Principle Diagnosis on Admission: | ||
| Secondary Diagnosis: | ||
| Allergies: | ||
| Medications ADDED this visit: (begin taking these) |
Medications CHANGED this visit: (modify what you were taking) |
Medications STOPPED this visit: (stop taking these) |
| Final Discharge Medication List | |||||
| Medication/Route/Dosage/Frequency/Duration | Comments | Morning | Afternoon | Evening | Bedtime |
| As Needed Medications | |||||
Medication Reconciliation - Finalized Medication List
| Patient Name: Stone, Mitchel | Date of Birth: 3/21/1940 | Room: 805 |
| Medication (name/strength) | Dose | Route | Frequency | Notes |