- Admissions
- Order Review
- Product Dispensing
- Verification
- Clinical Services
- Drug Info
| King, Whitney |
| MRN: 200536 | Room: 522 | DOB: 4/17/1975 | Age: 51 | Gender: Female | Allergies: NKDA |
| Setting | Adult Medicine Unit | ||
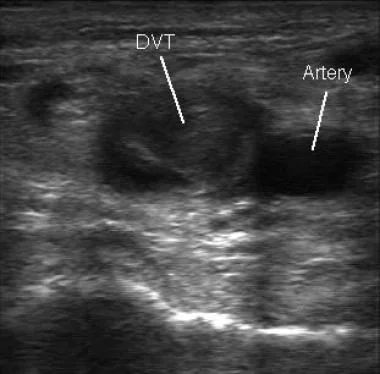
| Scenario | Today, you are on rounds with the Internal Medicine team outside the room of a patient who was admitted from the emergency department for management of an acute DVT. | ||
| Admission note taken on 01/31/26 | |||
| CC | pain and swelling of her left lower extremity | ||
| HPI | A patient with a history or coronary artery disease and angine reports that in frustration over angina associated with moderate physical activity, she decided to spend the weekend in bed reading and watching television. This morning she awakened with significant pain and swelling of her left lower extremity, which on inspection is warm and erythematous. She presented to the emergency room, and a duplex ultrasound was postive fer deep vein thrombosis. | ||
| PMH |
|
||
| Social History |
|
Family History |
|
| Vaccine History |
None on file | Surgical History |
None on file |
| Physical Exam |
|
||
Clinical Laboratory Report
| Test Name | 02/01/26 | 01/31/26 | Range |
| Sodium (Na+) | 137 | 141 | 136-145 mEq/L |
| Potassium (K+) | 4.8 | 4.7 | 3.5-5 mEq/L |
| Chloride (Cl-) | 96 | 93 | 98-106 mEq/L |
| Bicarbonate (HCO3-) | 26 | 25 | 23-28 mEq/L |
| Urea nitrogen (BUN) | 14 | 14 | 8-20 mg/dL |
| Creatinine | 0.7 | 0.7 | 0.5-1.3 mg/dL |
| Glucose | 82 | 84 | 70-115 mg/dL |
| Hemoglobin A1c | 5.5 | 5.3-7.5 % | |
| Calcium,Total | 9.2 | 8.9 | 8.6-10.2 mg/dL |
| Phosphate | 4.1 | 4 | 3-4.5 mg/dL |
| Magnesium | 1.9 | 1.9 | 1.6-2.6 mEq/L |
| Protein, total | 7.2 | 7.2 | 5.5-9 g/dL |
| Albumin | 4.3 | 4.3 | 3.5-5.5 g/dL |
| Aminotransferase,aspartate (AST) | 16 | 16 | 10-40 units/L |
| Aminotransferase,alanine (ALT) | 12 | 12 | 10-40 units/L |
| Lactic dehydrogenase (LDH) | 84 | 83 | 80-225 units/L |
| Alkaline phosphatase | 74 | 75 | 30-120 units/L |
| Bilirubin, Total | 0.7 | 0.7 | 0.3-1 mg/dL |
| Leukocytes (WBC) | 6.3 | 6.2 | 4.5-11 x103/mcL |
| Red blood cells (RBC), Female | 4.1 | 4.1 | 4.3-5.7 x108/mcL |
| Hemoglobin, Female | 14.8 | 14.5 | 12-16 g/dL |
| Hematocrit, Female | 38 | 38.4 | 37-47 % |
| Mean corpuscular hemoglobin (MCH) | 28 | 27 | 27-33 picogram |
| Mean corpuscular volume (MCV) | 89 | 88 | 76-100 mcm3 |
| Platelets | 362 | 360 | 150-450 x103/mcL |
| International normalized ratio (INR) | 1.7 | 1.0 | 0.8-1.2 |
| Prothrombin time (PT) | 18.8 | 14.2 | 9.5-11.3 sec |
| Partial thromboplastin time,activated (aPTT) | 68 | 28 | 25-35 sec |
| Additional Labs: |
|
||||||||||
| Cultures: | None | ||||||||||
| Imaging Studies: |
|
| ||||||||||||||||||||||||||||||||||||||||||
Current Orders
| Medication History |
|
Home Medication List: verified by pharmacy on admit (01/31/26)
| Patient Name: King, Whitney Date of Birth: 4/17/1975 Room#: 522 |
Allergies: |
Immunization History: |
| Community Rx Info: Rx Insurance: |
Social History: |
|
| Additional Notes: | ||
STRENGTH DF |
ROUTE FREQ |
DOSE (date/time) |
EFFECTS |
ACTION |
REASON |
|||
|---|---|---|---|---|---|---|---|---|
| Action Key: C = Continue, D = Discontinue*, H = Hold*, M = Modify* *must provide reason |
||||||||
| Medication | 02/01/26 | 01/31/26 |
| Heparin 1,400 units/hr IV continuous Rate: 14 mL/hr | 7:33 | 7:44 |
| Warfarin 10 mg PO QAM | 9:38 | 9:28 |
| Isosorbide dinitrate 80 mg PO Q6H | 00:46 6:38 12:15 | 00:26 6:53 12:46 18:51 |
| Aspirin EC 325 mg PO QD | 9:38 | 9:32 |
| Diltiazem CD 180 mg PO QD | 9:38 | 9:56 |
| Cimetidine 200 mg PO BID PRN PRN GERD | 9:57 | 9:50 21:42 |
| Heparin 6,000 units IV STAT x1 Rate: push over 2 minutes | 6:48 | 6:14 |
Clinical Notes
Medication Discharge Orders
Discharge Planning - Medication List and Instructions
| Hospital Medications | ||||||
| Medication | Instructions | Comments | Continue | Modify | Discontinue | New Rx sent |
| Previous Home Medications | ||||||
| Medication | Instructions | Comments | Continue | Modify | Discontinue | New Rx sent |
Discharge Planning - Medication List and Instructions
| Patient Name: | ||
| Admission Date: | Discharge Date: | Service: |
| Principle Diagnosis on Admission: | ||
| Secondary Diagnosis: | ||
| Allergies: | ||
| Medications ADDED this visit: (begin taking these) |
Medications CHANGED this visit: (modify what you were taking) |
Medications STOPPED this visit: (stop taking these) |
| Final Discharge Medication List | |||||
| Medication/Route/Dosage/Frequency/Duration | Comments | Morning | Afternoon | Evening | Bedtime |
| As Needed Medications | |||||
Medication Reconciliation - Finalized Medication List
| Patient Name: King, Whitney | Date of Birth: 4/17/1975 | Room: 522 |
| Medication (name/strength) | Dose | Route | Frequency | Notes |